Old way vs new way of measuring cholesterol
Most people are told they have “high cholesterol” without too much of a backdrop as to what that means or why it matters. In reality, cholesterol and the particles that carry it are not the same thing. Understanding that distinction is key to understanding why modern markers like ApoB are gaining attention alongside traditional cholesterol tests.
This article explains:
-
What cholesterol actually is
-
What lipoproteins do and why they matter
-
The traditional (“old way”) cholesterol markers
-
The newer particle-based approach using ApoB
-
How these measures work best together
First, what is cholesterol?
Cholesterol is a fat-like molecule that plays essential roles in the body. It is used to:
-
Build cell membranes
-
Produce steroid hormones
-
Make vitamin D
-
Support bile acid production for digestion
Your body makes most of the cholesterol it needs in the liver. Some also comes from food.
The important point is this: Cholesterol is not harmful by default. Problems arise when cholesterol ends up in the wrong place, particularly inside artery walls.
What is a lipoprotein, and why do we need them?
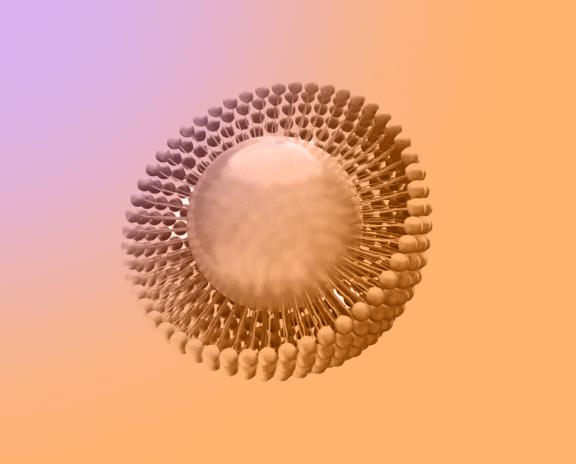
Blood is mostly water. Cholesterol and fats do not dissolve in water. To move cholesterol safely through the bloodstream, the body packages it into lipoproteins. These are microscopic transport particles made of fat and protein.
Think of it like this:
-
Cholesterol is the cargo
-
Lipoproteins are the vehicles (or boats!)
Different lipoproteins carry cholesterol in different directions and behave differently in the circulation. This is why cholesterol testing is really about lipoproteins, not cholesterol alone.
The old way: traditional cholesterol markers
The traditional lipid panel focuses on how much cholesterol is carried, rather than how many particles are carrying it. These tests remain the backbone of NHS cardiovascular risk assessment.
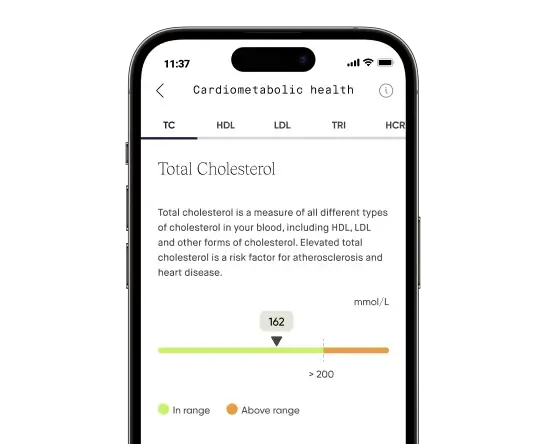
Total cholesterol
Total cholesterol is the combined amount of cholesterol carried by all lipoproteins.
It is useful for screening, but it does not show how cholesterol is distributed between protective and harmful particles.
LDL cholesterol (LDL-C)
LDL cholesterol reflects how much cholesterol is carried inside low-density lipoprotein particles.
LDL-C:
-
Is a central target in UK and European guidelines
-
Is strongly associated with cardiovascular events
-
Responds well to lifestyle changes and statins
Its limitation is that it measures cholesterol mass, not particle number.
Related page: LDL cholesterol biomarker page | Blood test (UK only)
HDL cholesterol (HDL-C)
HDL cholesterol measures cholesterol carried by high-density lipoproteins, which help remove excess cholesterol from artery walls.
Higher HDL is generally associated with lower risk, but:
-
HDL function matters as much as amount
-
Very high HDL is not always protective
Related page: HDL cholesterol biomarker page | Blood test (UK only)
HDL % of total cholesterol
This calculated marker shows how much of your total cholesterol comes from HDL.
It provides a simple view of lipid balance and can highlight unfavourable patterns even when total cholesterol appears acceptable.
Related page: HDL % of total cholesterol | Blood test (UK only)
The limitation of the old way
Two people can have the same LDL cholesterol but very different cardiovascular risk. Why?
Because:
-
LDL-C tells you how much cholesterol is inside LDL particles
-
It does not tell you how many LDL-like particles are circulating
More particles means more opportunities for cholesterol to enter artery walls over time.
This limitation becomes especially relevant in people with:
-
Insulin resistance or metabolic syndrome
-
High triglycerides
-
Fatty liver disease
-
A strong family history of early heart disease
The new way: ApoB and particle counting
What ApoB measures
Apolipoprotein B (ApoB) is a structural protein found on all atherogenic lipoproteins, including:
-
LDL
-
VLDL
-
IDL
-
Lipoprotein(a)
Each of these particles carries exactly one ApoB molecule.
That makes ApoB a direct count of plaque-driving particles, not a measure of how much cholesterol they contain.
Related page: ApoB blood biomarker | Blood test (UK only)
Why ApoB matters
Cardiovascular risk is driven by how often artery walls are exposed to atherogenic particles over time. Large genetic studies, population cohorts, and meta-analyses consistently show that:
-
ApoB predicts cardiovascular events better than LDL-C
-
Reducing ApoB reduces heart attack and stroke risk
-
LDL-C and ApoB can be “discordant”, revealing hidden risk
This particle-based view has been adopted by many preventive cardiologists, who focus on cumulative lifetime exposure rather than short-term thresholds.
Old way vs new way: comparison table
|
Marker |
What it measures |
What it tells you |
Main limitation |
|
Total cholesterol |
Cholesterol content |
Broad screening |
No particle insight |
|
LDL-C |
Cholesterol in LDL |
Treatment guidance |
Misses particle count |
|
HDL-C |
Cholesterol in HDL |
Protective context |
Function not measured |
|
HDL % |
Balance of cholesterol |
Ratio insight |
Still cholesterol-based |
|
ApoB |
Particle number |
True atherogenic burden |
Less widely ordered |
NHS perspective vs modern prevention
The NHS approach prioritises:
-
Cost-effective population screening
-
LDL-C and non-HDL cholesterol
-
Risk calculators to guide treatment
This works well for most people. The modern prevention approach asks:
“How many atherogenic particles has this person been exposed to over a lifetime?”
ApoB helps answer that question, especially when standard cholesterol tests underestimate risk.
Crucially, this is not a replacement model. The strongest assessments combine LDL-C, non-HDL cholesterol, ApoB, inflammatory markers, and metabolic context.
FAQs
Is cholesterol itself bad?
No. Cholesterol is essential. Risk depends on where it ends up and how often artery walls are exposed to cholesterol-carrying particles.
Is LDL cholesterol outdated?
No. LDL-C remains clinically useful. ApoB adds precision rather than replacing it.
Can ApoB be high when LDL looks normal?
Yes. This is common in insulin resistance and high triglyceride states and can signal higher risk.
Should everyone measure ApoB?
Not necessarily. ApoB is most helpful when risk is unclear, underestimated, or treatment response needs refining.
The bottom line
Cholesterol is the cargo. Lipoproteins are the vehicles. Traditional tests measure how much cholesterol is being carried. ApoB measures how many vehicles are on the road.
Used together, these markers provide a clearer, more personalised picture of cardiovascular risk — without abandoning the evidence-based foundations of NHS care.